Журнал «Почки» Том 12, №4, 2023
Вернуться к номеру
Психосоматичні аспекти нефрологічної патології (огляд літератури)
Авторы: Безрук В.В. (1), Іванов Д.Д. (2), Шкробанець І.Д. (3), Джаббарлі І. (2)
(1) — Буковинський державний медичний університет, м. Чернівці, Україна
(2) — Національний медичний університет імені О.О. Богомольця, м. Київ, Україна
(3) — Національна академія медичних наук України, м. Київ, Україна
Рубрики: Нефрология
Разделы: Справочник специалиста
Версия для печати
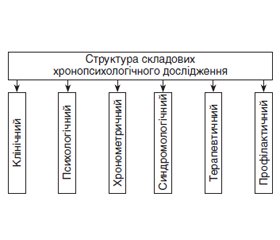
У статті наведено аналіз теоретичних і практичних результатів досліджень щодо комплексного вивчення проблеми виникнення і розвитку психосоматичних розладів, зокрема в пацієнтів з нефрологічною патологією (сечостатева система). У статті приділяється увага питанням вегетативних дисфункцій і можливості використання хронопсихологічного прогнозування розвитку психосоматичних розладів у пацієнтів із нефрологічною патологією.
The article provides an analysis of theoretical and practical results of comprehensive studies on the problem of the emergence and development of psychosomatic disorders, in particular, in patients with renal pathology (genitourinary system). The article focuses on the issues of autonomic dysfunctions and the possibility of using chronopsychological prediction of psychosomatic disorders in patients with renal pathology.
психосоматичний розлад; сечостатева система; огляд
psychosomatic disorder; genitourinary system; review
Для ознакомления с полным содержанием статьи необходимо оформить подписку на журнал.
- Margraf J., Lavallee K., Zhang X.C., Schneider S. Social rhythm and mental health: a cross-cultural comparison. PLoS One. 2016. 11(3). e0150312. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4783111/pdf/pone.0150312.pdf doi: 10.1371/journal.pone.0150312.
- Omelchenko Y.М. Importance of the types of significant adults’ stress responses for development of personal stress tolerance. Psychological Journal. 2019. 5(12). 169-81. doi: 10.31108/1.2019.5.12.11.
- Denisenko T. How did the war affect the health of Ukrainians? 2023. https://life.pravda.com.ua/health/2023/02/15/252874.
- Slabky G.O., Rogach I.M., Kachala L.O., Kachala T.V. Regarding the impact of the war with the Russian Federation on the state of health of the population of Ukraine. 2023. https://dspace.uzhnu.edu.ua/jspui/bitstream/lib/50630/1/%D0%A2%D0%B5%D0%B7%D0%B8%201%20%D0%A4%D0%9F%D0%9E.pdf.
- Kornatsky V.M., Mikhal’chuk VM, Dyachenko LO. The effects of stress on the development and course of diseases. World of Medicine and Biology. 2017. 1. 194-202. https://womab.com.ua/en/smb-2017-01/6536.
- Психосоматичні стани під час війни. Український медичний журнал. 2022. 5(151). 1-3. doi: 10.32471/umj.1680-3051.151.233846. https://umj.com.ua/wp/wp-content/uploads/
- 2022/11/WEB_Chasopis_151.pdf.
- Денова Л.Д., Іванов Д.Д., Андруневич Р.Р., КоржO.M., Красюк E.K. Нефрологічна допомога в умовах воєнного стану. Нирки. 2022. 11(3). 122-135. doi: 10.22141/2307-1257.11.3.2022.372.
- Greenaway C., Fabreau G., Pottie K. The war in Ukraine and refugee health care: considerations for health care providers in Canada. CMAJ. 2022 Jul 11. 194(26). E911-E915. doi: 10.1503/cmaj.220675.
- Piccoli G.B., Brunori G., Gesualdo L. et al. The impact of the Russian-Ukrainian war for people with chronic diseases. Nat. Rev. Nephrol. 2022. 18(7). 411-412. doi: 10.1038/s41581-022-00574-z.
- Ivanov D.D. Organization of the specialized medical care in conditions of limited resources (military status) (on the example of the provision of nephrology aid in Ukraine). Нирки. 2023. 12(2). 42-48. doi: 10.22141/2307-1257.12.2.2023.404.
- Hamrahian S.M., Falkner B. Hypertension in Chronic Kidney Disease. Adv. Exp. Med. Biol. 2017. 956. 307-325. doi: 10.1007/5584_2016_84.
- Lv J.C., Zhang L.X. Prevalence and Disease Burden of Chronic Kidney Disease. Adv. Exp. Med. Biol. 2019. 1165. 3-15. doi: 10.1007/978-981-13-8871-2_1.
- Caplin B., Yang C.W., Anand S., Levin A., Madero M., Saran R. et al.; International Society of Nephrology’s International Consortium of Collaborators on Chronic Kidney Disease of Unknown Etiology (i3C). The International Society of Nephrology’s International Consortium of Collaborators on Chronic Kidney Disease of Unknown Etiology: report of the working group on approaches to population-level detection strategies and recommendations for a minimum dataset. Kidney Int. 2019 Jan. 95(1). 4-10. doi: 10.1016/j.kint.2018.08.019.
- Lameire N.H., Levin A., Kellum J.A., Cheung M., JadoulM., Winkelmayer W.C., Stevens P.E. Conference Participants. Harmonizing acute and chronic kidney disease definition and classification: report of a Kidney Disease: Improving Global Outcomes (KDIGO) Consensus Conference. Kidney Int. 2021 Sep. 100(3). 516-526. doi: 10.1016/j.kint.2021.06.028.
- Rao I.R., Bangera A., Nagaraju S.P., Shenoy S.V., PrabhuR.A., Rangaswamy D., Bhojaraja M.V. Chronic kidney disease of unknown aetiology: A comprehensive review of a global public health problem. Trop. Med. Int. Health. 2023 Aug. 28(8). 588-600. doi: 10.1111/tmi.13913.
- Steinberg H., Herrmann-Lingen C., Himmerich H. Johann Christian August Heinroth: psychosomatic medicine eighty years before Freud. Psychiatr. Danub. 2013 Mar. 25(1). 11-6. PMID: 23470601.
- Strengthening people-centred health systems in the WHO European Region: framework for action on integrated health services delivery. 2016. https://www.euro.who.int/__data/assets/pdf_file/0004/315787/66wd15e_FFA_IHSD_160535.pdf.
- 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice: Developed by the Task Force for cardiovascular disease prevention in clinical practice with representatives of the European Society of Cardiology and 12 medical societies With the special contribution of the European Association of Preventive Cardiology (EAPC). European Heart Journal. 2021. 42(34). P. 3227-3337. https://doi.org/10.1093/eurheartj/ehab484.
- Moroz G.Z., Holovanova I.A., Bychkova S.A., DzyzinskaO.O. Current aspects of engaging patients to shared decision-making and partner participation in the treatment process (review). Clinical and Preventive Medicine. 2023. 2(24). 89-98. doi: https://doi.org/10.31612/2616-4868.2(24).2023.13.
- Beaver N.A., Koch G.D., Waltz J.A., Konski A.F. Personalized Medicine: Insights Into Current Legal Issues. Personalized Medicine Bulletin. 2016. https://www.foley.com/en/insights/publications/2016/09/personalized-medicine-insights-into-current-legal.
- Організаційно-правові та соціально-економічні засади функціонування системи громадського здоров’я в Україні. 2021. 193 с. http://repository.pdmu.edu.ua/bitstream/123456789/16305/1/Osnovni_operativni_funkcii.pdf.
- Braig Z.V. Personalized medicine: From diagnostic to adaptive. Biomed J. 2022 Feb. 45(1). 132-142. doi: 10.1016/j.bj.2019.05.004. Epub 2019 Jul 9. PMID: 35590431; PMCID: PMC9133264.
- Mattsson B., Mattsson M. The concept of “psychosomatic” in general practice. Reflections on body language and a tentative model for understanding. Scand. J. Prim. Health Care. 2002 Sep. 20(3). 135-8. doi: 10.1080/028134302760234564. PMID: 12389748.
- Kokun O.M. Optimization of adaptive human capabilities: psychophysiological aspect ensuring activity. 2004. 264 р. https://lib.iitta.gov.ua/1513/1/%D0%9A%D0%BE%D0%BA%D1%83%D0%BD_%D0%9C%D0%BE%D0%BD%D0%BE%D0%B3%D1%80_04.pdf.
- Kolomoiets M.Y., Pavliukovych N.D., Khodorovskyi V.M., Tkach Y.P. Theories and conceptions of psychosomatic disorders. Buk. Med. Herald. 2008. 1(12). 141-144. https://core.ac.uk/download/pdf/144949486.pdf.
- Herzog W., Schneider A. Brücken von der Psychosomatik zur Allgemeinmedizin. Psychother. Psychosom. Med. Psychol. 2017 May. 67(5). 181-182. German. doi: 10.1055/s-0043-107273. Epub 2017 May 10. PMID: 28493243.
- Linden M., Muschalla B., Noack N., Heintze C., Doepfmer S. Treatment Changes in General Practice Patients With Chronic Mental Disorders Following a Psychiatric-Psychosomatic Consultation. Health Serv. Res. Manag. Epidemiol. 2018 Mar 15. 5. 2333392818758523. doi: 10.1177/2333392818758523. PMID: 29568790; PMCID: PMC5858609.
- Somatopsychic and psychosomatic disorders in the practice of an internist: bronchial asthma as a model of somatopsychiatry. Health-ua.org. http://www.health-ua.org/faq/depressiya-psihoterapiya/981.html.
- Bransfield R.C., Friedman K.J. Differentiating Psychosomatic, Somatopsychic, Multisystem Illnesses, and Medical Uncertainty. Healthcare (Basel). 2019 Oct 8. 7(4). 114. doi: 10.3390/healthcare7040114. PMID: 31597359; PMCID: PMC6955780.
- Budnik T.V. The importance of correction of autonomic dysfunction in children with urinary disorders or How to improve the efficacy of neurogenic bladder therapy. Child’s health. 2019. 14(1). 25-29. doi: 10.22141/2224-0551.14.1.2019.157875.
- МКХ-10 (ICD-10). https://e-mis.com.ua/mkx-10.
- Mazurak N., Enck P., Muth E., Teufel M., Zipfel S. Heart rate variability as a measure of cardiac autonomic function in anorexia nervosa: a review of the literature. Eur. Eat Disord. Rev. 2011 Mar-Apr. 19(2). 87-99. doi: 10.1002/erv.1081. Epub 2010 Dec 28. PMID: 25363717.
- van der Kruijs S.J., Vonck K.E., Langereis G.R., Feijs L.M., Bodde N.M., Lazeron R.H. et al. Autonomic nervous system functioning associated with psychogenic nonepileptic seizures: Analysis of heart rate variability. Epilepsy Behav. 2016 Jan. 54. 14-9. doi: 10.1016/j.yebeh.2015.10.014. Epub 2015 Nov 25. PMID: 26615481.
- Billeci L., Tonacci A., Brunori E., Raso R., Calderoni S., Maestro S., Morales M.A. Autonomic Nervous System Response during Light Physical Activity in Adolescents with Anorexia Nervosa Measured by Wearable Devices. Sensors (Basel). 2019 Jun 24. 19(12). 2820. doi: 10.3390/s19122820. PMID: 31238575; PMCID: PMC6630965.
- Schneider M., Schwerdtfeger A. Autonomic dysfunction in posttraumatic stress disorder indexed by heart rate variability: a meta-analysis. Psychol. Med. 2020 Sep. 50(12). 1937-1948. doi: 10.1017/S003329172000207X. Epub 2020 Aug 28. PMID: 32854795; PMCID: PMC7525781.
- Bilgi M.M., Vardar R., Yıldırım E., Veznedaroğlu B., Bor S. Prevalence of Psychiatric Comorbidity in Symptomatic Gastroesophageal Reflux Subgroups. Dig. Dis. Sci. 2017 Apr. 62(4). 984-993. doi: 10.1007/s10620-016-4273-4. Epub 2016 Aug 26. PMID: 27565506.
- Feng L., Li Z., Gu X., Jiang J., Liu X. Psychosomatic Disorders in Patients with Gastrointestinal Diseases: Single-Center Cross-Sectional Study of 1186 Inpatients. Gastroenterol. Res. Pract. 2021 May 1. 2021. 6637084. doi: 10.1155/2021/6637084. PMID: 34007268; PMCID: PMC8110399.
- Artemieva M.S., Kuznetsov V.I., Sturov N.V., ManyakinI.S., Basova E.A., Shumeyko D. Psychosomatic Aspects and Treatment of Gastrointestinal Pathology. Psychiatr. Danub. 2021 Spring-Summer. 33 (Suppl. 4). 1327-1329. PMID: 35503951.
- Fleischer M., Szepanowski F., Tovar M., Herchert K., DinseH., Schweda A. et al. Post-COVID-19 Syndrome is Rarely Associated with Damage of the Nervous System: Findings from a Prospective Observational Cohort Study in 171 Patients. Neurol. Ther. 2022 Dec. 11(4). 1637-1657. doi: 10.1007/s40120-022-00395-z. Epub 2022 Aug 26. PMID: 36028604; PMCID: PMC9417089.
- Stettner M., Fleischer M., Skoda E.M., Teufel M., Kleinschnitz C. Response Letter to Vink et al. Neurological Study Does Not Provide Any Evidence that Long COVID is Psychosomatic. Neurol. Ther. 2023 Feb. 12(1). 333-336. doi: 10.1007/s40120-022-00424-x. Epub 2022 Dec 12. PMID: 36508158; PMCID: PMC9744056.
- Vink M., Grande T., Kohl M. Letter to the Editor Regarding Fleischer et al. Neurological Study Does Not Provide Any Evidence that Long COVID is Psychosomatic. Neurol. Ther. 2023 Feb. 12(1). 329-332. doi: 10.1007/s40120-022-00426-9. Epub 2022 Dec 12. PMID: 36508159; PMCID: PMC9744047.
- Lugović-Mihić L., Ljubesić L., Mihić J., Vuković-CvetkovićV., Troskot N., Situm M. Psychoneuroimmunologic aspects of skin diseases. Acta Clin. Croat. 2013 Sep. 52(3). 337-45. PMID: 24558766.
- Peters E.M. Stressed skin? — a molecular psychosomatic update on stress-causes and effects in dermatologic diseases. J. Dtsch Dermatol. Ges. 2016 Mar. 14(3). 233-52; quiz 253. doi: 10.1111/ddg.12957. PMID: 26972185.
- Winkley K., Upsher R., Stahl D., Pollard D., Kasera A., Brennan A., Heller S., Ismail K. Psychological interventions to improve self-management of type 1 and type 2 diabetes: a systematic review. Health Technol. Assess. 2020 Jun. 24(28). 1-232. doi: 10.3310/hta24280. PMID: 32568666; PMCID: PMC7336224.
- Kampling H., Köhler B., Germerott I., Haastert B., IcksA., Kulzer B. et al. An Integrated Psychosomatic Treatment Program for People with Diabetes (psy-PAD). Dtsch Arztebl. Int. 2022 Apr 8. 119(14). 245-252. doi: 10.3238/arztebl.m2022.0094. PMID: 35074044; PMCID: PMC9358352.
- Sadowsky R.L., Sulejmani P., Lio P.A. Atopic Dermatitis: Beyond the Skin and Into the Gut. J. Clin. Med. 2023 Aug 25. 12(17). 5534. doi: 10.3390/jcm12175534. PMID: 37685600; PMCID: PMC10487925.
- Hoeritzauer I., Phé V., Panicker J.N. Urologic symptoms and functional neurologic disorders. Handb. Clin. Neurol. 2016. 139. 469-481. doi: 10.1016/B978-0-12-801772-2.00038-2. PMID: 27719863.
- Kuffel A., Kapitza K.P., Löwe B., Eichelberg E., Gumz A. Chronische Pollakisurie: Zystektomie oder Psychotherapie. Urologe A. 2014 Oct. 53(10). 1495-9. German. doi: 10.1007/s00120-014-3618-x. PMID: 25214314.
- Wuestenberghs F., Baron M., Melchior C., Desprez C., Cornu J.N., Leroi A.M., Gourcerol G. Overlaps with bladder pain syndrome and irritable bowel syndrome are associated with higher symptom burden and reduced quality of life in functional dyspepsia. Neurogastroenterol. Motil. 2022 Nov. 34(11). e14414. doi: 10.1111/nmo.14414. Epub 2022 May 24. PMID: 35608061.
- Domenici L., Perniola G., Giorgini M., Lecce F., Bracchi C., Musella A. et al. Vulvodynia: current opinion and treatment strategies. Minerva Ginecol. 2016 Dec. 68(6). 727-32. Epub 2015 Jun 30. PMID: 26126068.
- Mullins C., Bavendam T., Kirkali Z., Kusek J.W. Novel research approaches for interstitial cystitis/bladder pain syndrome: thinking beyond the bladder. Transl. Androl. Urol. 2015 Oct. 4(5). 524-33. doi: 10.3978/j.issn.2223-4683.2015.08.01. PMID: 26813921; PMCID: PMC4708560.
- Seleznova I.В., Storozhuk L.О., Dovgaliuk T.V. Psychosomatic disorders in patients with chronic kidney disease. Ukrainian Journal of Nephrology and Dialysis. 2017. 3(55). 9-11.
- Іванов Д.Д. Організація спеціалізованої медичної допомоги в умовах обмежених ресурсів (військовий стан) (на прикладі надання нефрологічної допомоги в Україні). Нирки. 2023. 12(2). 42-50.
- Sever M.S., Vanholder R., Luyckx V., Noruišiene E., TuglularS. Armed conflicts and kidney patients: a consensus statement from the Renal Disaster Relief Task Force of the ERA. Nephrology Dialysis Transplantation. 2023. 38(1). Р. 56-65. https://doi.org/10.1093/ndt/gfac247.
- Савенкова І.I. Хронопсихологічне прогнозування перебігу захворювань у психосоматичних хворих. Київ, 2014. 320 с. https://elibrary.kubg.edu.ua/id/eprint/5664/1/I_Savenkova_M_KSPKIO_IL.pdf.