Журнал «Боль. Суставы. Позвоночник» 4 (08) 2012
Вернуться к номеру
The Importance of Quantitative Ultrasound in the Early Detection and Management of Osteoporosis. Can we adopt the QUS ISCD Position Statements to the Omnisense QUS series?
Авторы: Didier Hans, Center of Bone diseases, Bone and Joint Department, Lausanne University Hospital, Lausanne Switzerland
Рубрики: Ревматология, Травматология и ортопедия
Разделы: Новости
Версия для печати
/72/72.jpg) Key messages
Key messages
ISCD published position statements on heel QUS devices in 1997 follow-up by an update in 2010. The objective of this short head to head review was to see, if based on selective literatures search, one can extrapolated with sufficient level of confidence the QUS ISCD Position statements to the Omnisense QUS series and if the claims of the manufacturer in regards to the use of their devices are reasonable. In summary:
— SOS measurements provide a more complete picture of the bone’s fragility than Bone mineral density alone as assessed by DXA.
— Non-heel axial transmission QUS can discriminate those with osteoporotic fractures from age-matched controls without osteoporotic fracture.
— Discordant results between radius/tibia/phalanx QUS and central DXA, which are not infrequent, are not necessarily an indication of methodological error.
— From the latest prospective study, Radius and Tibia SOS estimate sufficiently the prediction of fragility fracture in postmenopausal women to be used in conjunction with clinical risk factors.
– QUS in conjunction with clinical risk factors can be used to identify a population at very low fracture probability in which no further diagnostic evaluation may be necessary.
– If central DXA cannot be done, pharmacologic treatment can be initiated if the fracture probability, as assessed by QUS using device specific thresholds and in conjunction with clinical risk factors, is sufficiently high.
— QUS cannot be used to monitor the skeletal effects of treatments for osteoporosis. Normal bone status follow-up in the postmenopausal period is however doable.
Rational
According to the internationally accepted definition, osteoporosis is a progressive systemic skeletal disease characterized by a low bone mass and micro architectural deterioration of bone tissue, with a consequent increase in bone fragility and susceptibility to fracture [1]. Osteoporotic fractures and specifically hip fractures increase dramatically with age and are responsible for considerable mortality. Therefore it is accepted as a major public health problem with huge associated cost. However, many studies have been conducted in the field of osteoporosis over the last two decades and several treatments have proven effective for the reduction of fracture risk and/or bone mineral density increase.
Osteoporosis is currently diagnosed by the occurrence of a low trauma vertebral or hip fracture (clinical diagnosis), or by measurement of bone mineral density as assessed by dual-energy X-ray absorptiometry (DXA) according to the World Health Organization (WHO) criteria [1].
Today at least two major challenges remain. The first is still related to the awareness to the disease or at least turning awareness into action. Indeed, from an International Osteoporosis Foundation (IOF) report, more than 70 % of the people at risk of osteoporosis have never been diagnosed nor screened [2]. This problem might be different depending on the countries (for example Europe versus Asia) but the overall aging of the population will amplify this phenomenon. The second major challenge is to better identify individuals at high risk of fracture who would benefit from intervention. Indeed, bone density is one of the major determinants of bone strength and fracture risk, but it is not the only determinant/clinical risk factors (CRF), and considerable overlap exists in BMD values between individuals who develop fragility fractures and those who do not [3]. It is therefore of major importance to improve our strategy in detecting patients at high risk of fracture, who will benefit from treatments.
In practice, central DXA is unfortunately not universally available and in addition, currently raised reimbursement issues in many countries will not help the spreading of this technique [4]. In many countries, bone specialists use other available technologies, such as Quantitative Ultrasound (QUS), peripheral DXA, hand X-ray, or clinical judgment.
The introduction of quantitative ultrasound (QUS) applicable to different and peripheral skeletal sites [5], along with the absence of technology-specific guidelines, have created great uncertainty in applying the results of such technique to managing individual patients in clinical practice. Yet, QUS has several advantages over DXA, in early detection: Its lower cost, size, portability, operation cost, the lack of the need for a roentgen technician and a special room, and the lack of ionizing radiation lends to greater availability especially in the developing world or where DXA reimbursement become an issue. The International Society for Clinical Densitometry (ISCD) addressed these uncertainties (clinical applications of QUS for fracture risk assessment, diagnosis of osteoporosis, treatment initiation, monitoring of treatment, and quality assurance/quality control) in 2007 in its Official Positions on the appropriate clinical application of QUS, based on a review of the relevant evidence at that time [6], and has adapted these recommendations for use in the Asia-Pacific region [7]. These recommendations were further evidenced in the 2010 ISCD — IOF FRAX initiative [8] and in a meta-analysis just published recently on 55,164 women and 13,742 men [9]. However these statements were focused mostly on Heel QUS devices.
The objective of this short head to head review is to see, if based on selective literatures search, one can extrapolated with sufficient level of confidence the QUS ISCD Position statements to the Omnisense QUS series (BeamMed Ltd, Israel) and if the claims of the manufacturer in regards to the use of their devices are reasonable.
Technological diversity amongst QUS devices
— For QUS, bone density measurements from different devices cannot be directly compared (ISCD Official Position [6]).
Technological diversities amongst QUS devices are not a new concept in the medical field. Indeed, while DXA is the gold standard for the diagnosis of osteoporosis, there are major differences among manufacturers and models. As a result, absolute value of BMD, the common parameter for all DXA devices, cannot be compared with different manufacturers and models. It is usual to categorize DXA into fan, pencil or cone beam X-ray devices. The degree of technical diversity of QUS devices and parameters is much larger than what is commonly found in DXA. This increases the difficulties in comparing measurements with different QUS devices and may lead to misinterpretation of results. Therefore direct comparison of the QUS devices cannot be performed without significant bias, i.e., results from one QUS device cannot be extrapolated to another one that is technologically different. This statement is also true for the Omnisense QUS devices.
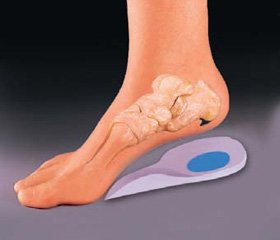
The Sunlight Omnisense/Mini Omni Ultrasound Bone Sonometers are the first non-invasive ultrasound device capable of measuring bone speed of sound (SOS) at one or more skeletal sites. It is comprised of a Main Unit and small hand held probes, each designed to measure SOS at one or more specific skeletal sites such as the distal one-third of the radius, the proximal third phalanx, the fifth metatarsal and the mid-shaft tibia. All types of Sunlight Omnisenses measures SOS utilizing a technology based on well-established laws of physics (Ultrasound Critical Angle Propagation Chronometry) applied to the transmission of signals along the bone [10–13]. However it is important to note that no significant difference was found between the different Sunlight QUS models [14] when comparing the same skeletal sites. Nevertheless, as for DXA, one cannot expect forcedly to have the same results between skeletal sites (e.g. radius versus Tibia).
It has been shown that SOS provides a measure of skeletal fragility [10–13]. Indeed from these different papers it appears clearly that SOS at the radius or at the tibia is related to cortical thickness, cortical density as well as to some extent to its porosity. When we have a thin cortical shell in reference to the wavelength, then, the ultrasound waves will also travel in the trabecular bone layer immediately under the cortical shell. In addition, results suggest that different axial transmission approaches give access to different bone mechanical parameters (e.g. failure load). The association of different axial transmission techniques should be able to provide a good prediction of bone mechanical parameters, and should therefore be helpful for fracture risk prediction.
In conclusion, SOS measurements reflect several varied bone properties, such as density, elasticity, cortical thickness, and to a smaller extent micro-architecture, thus providing a more complete picture of the bone’s fragility than Bone mineral density alone as assessed by DXA.
Can QUS be used for fracture risk assessment?
— The only validated skeletal site for the clinical use of QUS in osteoporosis management is the heel (ISCD Official Position [6]).
This statement has been made couple years ago as at that time because of the insufficient number of publications for non-heel QUS devices. Since then, things changed substantially with more than 60 publications on Omnisense QUS devices on fracture discriminations [15–30], fracture prediction [31–34], age related changes [35–37], screening strategy [38–41], bone status follow-up with- without treatment [42–48], secondary osteoporosis [49–52], etc.
— Validated heel QUS devices predict fragility fracture in postmenopausal women (hip, vertebral and global fracture risk) and men over the age of 65 (hip and all non-vertebral fractures), independently of central DXA BMD (ISCD — IOF Official Position [6, 8]).
— For QUS, different devices should be independently validated for fracture risk prediction by prospective trials or by demonstration of equivalence to a clinically validated device (ISCD Official Position [6]).
— Discordant results between heel QUS and central DXA are not infrequent and are not necessarily an indication of methodological error (ISCD Official Position [6]).
It is becoming well established that overall, non-heel axial transmission QUS can discriminate those with osteoporotic fractures (hip, spine, any osteoporotic fracture) from age-matched controls without osteoporotic fracture [15–30]. Most of these studies outcome, although slightly less sensitive than heel ultrasound, were independent of BMD and age and demonstrated that the combination of QUS and BMD measurements may improve the accuracy of identification of women who will sustain a fracture.
The power of non-heel axial transmission QUS to predict fracture observed in cross-sectional studies has been confirmed by some but not all prospective studies [31–34]. Indeed, the first prospective study by Lee S.H. et al. [33] failed to demonstrate the ability of Radius and Tibia SOS to predict prospectively osteoporotic fracture. However this study has a major limitation related to a too large age difference between groups which could not be entirely adjusted by statistics explaining these partially negative results. A previous attempt was done by Dobnig et al. [31], but in a population of elderly women living in nursing homes Whereas incident hip and non-vertebral fracture risk was related to Achilles+ SI (HR 1.3 (1.1–1.4), respectively 1.1 (1.02–1.3)), Omnisense SOS phalange or radius was not predictive of fracture. But again the sample size was very small and the studied population very specific. In fact even the Achilles+ showed borderline results about twice as low as usually reported in the literatures. The most important positive and robust results are coming from a large prospective study from Canada [34]. The purpose of this prospective investigation was to assess the ability of Beam-Med (previously Sunlight) Omnisense quantitative ultrasound (QUS) to predict fractures over a five year follow-up period. A total of 1108 men and 2633 women were assessed with QUS at the tibia, radius and phalanx sites as part of the Canadian Multicenter Osteoporosis Study. A total of 204 fractures were recorded over the follow-up period. When all fractures were considered, an increase of 150 m/s in the SOS measure was associated with a decrease of fracture risk by 25 % when measured at the radius (HR = 0.746, p < 0.001), by 30 % when measured at the tibia (HR = 0.701, p < 0.001) and by 7 % when measured at the phalanx (HR = 0.929, NS). When fractures were limited to only non-vertebral fractures (187 fractures), an increase in the SOS by 150 m/s was associated with a decrease in fracture risk by 26 % when measured at the radius (HR = 0.743, p < 0.001), by 30 % when measured at the tibia, and by 8 % when measured at the phalanx (HR = 0.923, NS). At the radius and tibia sites a change in SOS by approximately one standard deviation was associated with a 25–30 % change in five-year fracture risk. The Authors concluded that the Beam-Med Omnisense multisite ultrasound has demonstrated to be a valuable tool for fracture risk assessment. One has to keep in mind that as for heel QUS device, discordant results between radius/tibia/phalanx QUS and central DXA, which are not infrequent, are not necessarily an indication of methodological error but rather due to the independence between the two techniques.
In conclusion, all these studies showed contrasted (mostly positive) results about the positiveness of the Omnisense at difference skeletal sites. However from the latest prospective study, Radius and Tibia SOS (but not the phalanges) estimate sufficiently the prediction of fragility fracture in postmenopausal women (hip, vertebral and global fracture risk) to be used in conjunction with clinical risk factors. Additional studies would be needed for the phalanges to further strengthen these conclusions using either a prospective study and/or another large population based study.
Can QUS be used to diagnose osteoporosis?
— The WHO diagnostic classification cannot be applied to T-scores from measurements other than DXA at the femur neck, total femur, lumbar spine or one-third (33 %) radius because those T-scores are not equivalent to T-scores derived by DXA (ISCD Official Position [6]).
This statement is perfectly applicable to the Omnisense devices as well. Indeed, The WHO classification of BMD was established using central DXA technologies at specified skeletal sites with a female postmenopausal Caucasian reference database [1]. It is not possible to apply the WHO criteria to other technologies and other skeletal sites. The WHO T-score range of –2.5 or less identifies approximately 30 % of postmenopausal women as having osteoporosis, which also approximates the average lifetime risk of osteoporotic fractures (clinical spine fracture, hip and forearm). The T-score diagnostic threshold of –2.5 cannot be applied to QUS devices without the risk of having discrepancies in the number of women diagnosed with osteoporosis.
From this variation and because of the intrinsic origin of the WHO classification of osteoporosis, one cannot use this definition for other sites than BMD of the femur, spine and 1/3 radius.
In conclusion, WHO classification criteria for osteoporosis as developed for DXA measurement of the spine, Femur and 1/3 radius cannot be applied to QUS measurement although the Weiss studies [17, 35] are rather opposite to that. Omnisense device specific thresholds could be calculated and be used in a triage approach as suggested in the next paragraph.
Can QUS be used to initiate treatment or further evaluation?
— Central DXA measurements at the spine and femur are the preferred method for making therapeutic decisions and should be used if possible. However, if central DXA cannot be done, pharmacologic treatment can be initiated if the fracture probability, as assessed by heel QUS using device specific thresholds and in conjunction with clinical risk factors, is sufficiently high (ISCD Official Position [6]).
Available therapeutic intervention thresholds vary due to either the presence or absence of clinical risk factors (CRFs) for fracture or different CRFs being used as a function of the professional group that are suggesting the recommendations. It is generally accepted that the BMD threshold for initiating treatment is higher when CRFs are present. It is also well-established that the basic parameters associated with QUS measurement of bone, namely the SOS, are associated with overall bone strength [10–13]. Bone strength is related to bone density, bone architecture (macro and micro) bone turnover, as well as the degree of bone mineralization. It is likely that these factors work together in an integrated way to maintain the overall quality and strength of bone to perform its function while preserving its integrity and its resistance to fractures. A key clinical question is whether individuals identified by QUS as «high-risk» for fracture will benefit significantly by treatment with antiresorptive agents or other specific medications against osteoporosis. Currently, there are no randomized clinical trials showing reduction of fracture risk in patients selected for treatment according to QUS measurement. But we have to face a certain paradox: treatment with approved antiresorptive drugs is associated with a reduction in fracture risk that is disproportionately greater than the increase in BMD, as determined by DXA. In other words, osteoporosis medications improve bone strength in ways that are not entirely dependent on BMD. Given the strong and positive relationship between QUS parameters and bone strength, it is unlikely that bone strength will increase under treatment with decreasing QUS values.
— Heel QUS in conjunction with clinical risk factors can be used to identify a population at very low fracture probability in which no further diagnostic evaluation may be necessary (ISCD Official Position [6]).
With the ability of QUS of the tibia and radius to predict osteoporotic fracture, and with the provision of central DXA being limited in some geographic areas, it has been suggested that QUS could be used in a triage mode. Indeed, one could define specific thresholds to identify patients at high or low risk of having osteoporosis. This approach has been proposed by the UK National Osteoporosis Society (NOS) for use with pDXA techniques and others [53, 54]. They have defined upper and lower values for pDXA parameters with 90% sensitivity (upper threshold) and 90% specificity (lower threshold) for identifying patients with central DXA T-score of –2.5 or lower at the hip or spine. At or above the threshold of 90% sensitivity, the likelihood of having osteoporosis was very low, with only 10 % of subjects being rated as false-negative. On the other hand, a specificity of 90 % could be used to define subjects as having high likelihood of osteoporosis. This leads to a low rate (10 %) of false-positive subjects. With such a triage approach the upper and lower thresholds are defined, specific to each QUS device and skeletal site, so that patients with osteoporosis by DXA of hip or spine are identified with 90% sensitivity and 90% specificity. Patients with a QUS result below the lower threshold are likely to have osteoporosis at the hip or spine; patients with a result above the upper threshold are unlikely to have osteoporosis, while those between the two thresholds require a hip and spine DXA BMD for a definitive diagnosis [6]. Nevertheless, it is difficult to define a «high-risk» threshold that will identify a patient who is likely to benefit from osteoporotic medication with a sufficient level of confidence. To partially solve this problem, we recommend requiring the presence of major CRFs in conjunction with low QUS parameters to make treatment decisions. The difficulty of applying CRFs to individual patients is the absence of quantitative values. Indeed, these parameters are usually categorical and the weight of each of them may vary. To overcome these difficulties, the calculation of an osteoporotic fracture probability taking into account the gradient of risk of QUS parameters and CRFs could replace a device-specific T-score. High- and low-risk probabilities then would help to determine the strategy for a given patient.
One can therefore project various scenarios:
1) in places where access to axial DXA is limited, because of financial and/or infrastructure issues, QUS could be used for treatment decisions independently of DXA and in conjunction with CRF;
2) in places where the awareness of osteoporosis is insufficient or where the number of axial DXA per habitants is not enough to cover the needs, QUS could be used in conjunction with clinical factors to establish the diagnosis in most cases [55], with DXA allocated for use to differentiate patients whose probability of fracture falls in the medium range; in this approach, QUS and CRF could be used to identify subjects at very low risk who do not need further evaluation as well subjects at very high risk for whom treatment initiation could be started (similarly to FRAX without BMD [56]). Any subject in the intermediate group of risk would be referred to additional test such as DXA. This approach seems to be aligned with the new 2007 ISCD recommendation [6].
Can QUS be used to monitor treatment?
— QUS cannot be used to monitor the skeletal effects of treatments for osteoporosis (ISCD Official Position [6]).
Monitoring treatment will depend of the precision of the device but also on the efficacy of such treatment at a given skeletal sites as well as a function of the magnitude of response. At present, there are very few studies evaluating the effects of pharmacological treatments on QUS parameters and clearly there is a lack of large randomized double-blind placebo-controlled studies. From the different studies listed previously [42–48], there is no clear evidence that QUS is even clinically useful in monitoring treatment. The best results are however related to HRT. Concerning the first one, as stated the clinical interest is limited as it is not even longitudinal. The second is much more exciting and could be used as such knowing that the main limitation is that it is an open label study with no real placebo group. Amazingly the Tibia SOS show good results for monitoring in comparison to the other skeletal site as assessed by QUS Omnisense but it still not surpasses the BMD measurement. Most importantly, for unclear reasons, current osteoporosis therapies are not always associated with measurable changes at peripheral skeletal sites depending on the region of interest and the device used. Whether this is a precision problem or simply a relative lack of treatment response at the peripheral site (or a combination of the two) remains unknown. As such it is not recommended for any type of QUS to monitor treatment in individual patients.
However theoretically, if a device is displaying a sufficiently good precision it should at least be able to monitor bone status over time. This is the case for the Omnisense Devices [15–48]. Indeed most of the studies reported in vivo precision inferior to 1 % as short or long term which appears to be very good. However one has to be careful in comparison precision between manufacturers. Indeed if we are looking for the SOS precisions for some of the heel ultrasound devices, they will be in the range of 0.3 %. These results are however completely misleading since it does not take into account the biological range of the parameters (e.g. the «bone loss» over life time as assessed by SOS). Therefore one would have to take into account the normative data biological range or as a surrogate, the standardized coefficient of variation (SCV%), using the following formula: root mean squared coefficient of variation (RMSCV) divided by (four times the standard deviations of the population divided by the mean of the population). When doing so, the standardized precision of the Omnisense is perfectly aligned with most of the good heel ultrasound devices.
In conclusion, although reported precision is usually very good, as today QUS cannot be used to monitor the skeletal effects of treatments for osteoporosis. Normal bone status follow-up in the postmenopausal period is however doable.
What should be in the QUS reporting?
— For QUS, the report should combine the following standard elements (ISCD Official Position [6]):
– Date of test, Demographics (name, date of birth or age, sex), Requesting provider, Names of those receiving copy of report, Indications for test, Manufacturer, and model of instrument and software version, Measurement value(s), Reference database, Skeletal site/region of interest, Quality of test, Limitations of the test including a statement that the WHO diagnostic classification cannot be applied to T-scores obtained from QUS measurements, Clinical risk factors, Fracture risk estimation, a general statement that a medical evaluation for secondary causes of low BMD may be appropriate.
— The report may include the following optional item (ISCD Official Position [6]):
– Recommendations for follow-up imaging
– Recommendations for pharmacological and non-pharmacological interventions.
Such a list is perfectly agreeable for any type of QUS devices and so it is for the Omnisense series.
What are the Quality Assurance and Quality Control (QA/QC) Criteria for QUS?
— For QUS, device-specific education and training should be given to the operators and interpreters prior to clinical use (ISCD Official Position [6]).
— Quality control procedures should be performed regularly (ISCD Official Position [6]).
Technical issues potentially affecting the utility of QUS include the dependence of measurements on temperature and acoustic coupling, the properties of soft tissues overlying bone and the absence of a universally accepted QUS phantom for cross-calibration between scanners. Manufacturer-specific phantoms exist but are not anthropomorphic, making quality control and cross-calibration among scanners challenging [57–59]. As the Omnisense is concerned [58], as today, when the device is turned on, the operator is instructed to perform a daily System Quality Verification measurement for each probe. This verification procedure is designed to test on a daily basis the accuracy status of the entire Omnisense system. The probe is placed on the surface of the phantom (using a contact ultrasound gel) and a standard type SOS measurement is performed. At the end of the measurement the operator is asked to enter the phantom’s temperature-corrected SOS (see below). A measurement history graph is then displayed, depicting a validity range around the expected temperature corrected values plus the measured points. Measurement history is shown, per operator’s choice, of the last month, last three months, last year or the entire history file. If for any reason the measurement value is outside the validity range, the operator is instructed to consult technical support. Each Omnisense (including MiniOmni) is supplied with a Perspex phantom. A thermometer strip is attached to the Perspex phantom, enabling a reading of the true phantom temperature. A conversion table attached to the phantom enables readout of the temperature-corrected phantom SOS. SOS readout tolerance is ±3 m/sec.
In conclusion, monitoring the performance and stability of the devices by regular temperature controlled quality control measurements using appropriate phantoms is a precondition for the assessment of good measurement quality. Also, QUS-specific training should be performed to raise the operator’s awareness to the specific requirements of QUS measurements. Indeed for most devices the operator has no influence over the study exam result after the signal has been recorded (i.e., no scan analysis).
Can QUS be used in children?
There is no ISCD Official Position on the use of QUS in children [60], mostly by lack of data at the time of the Consensus conference. However the concept that osteoporosis prevention begins during childhood is becoming increasingly accepted [60]. Bone fragility throughout the life cycle is determined in large part by bone density and geometry. Most pediatric bone studies have relied on DXA to assess bone mineral content and density. However, DXA provides areal bone mineral density (aBMD) measurements which, in children, are inherently biased by the size of the child, and have required software modifications due to the smaller size of the bones and surrounding soft tissue in younger children. In the field of pediatric bone research, peripheral Quantitative Computed Tomography (pQCT) is an imaging tool of increasing interest because of its ability to assess both density and geometry. Unlike DXA which is a two-dimensional imaging technique, pQCT provides authentic three-dimensional measures of trabecular and cortical density [61]. However, keeping in mind the issues related to the exposing children to ionizing radiation, a steady trend in QUS development from neonate to adolescent has been clearly seen. More than 20 papers have been published on the topic using the Omnisense QUS devices [62–90] and the majority of them carried out positive encouraging outcomes adjusted for gender, pubertal status etc. Today it might be difficult to extract a consensus on how to use it in clinical routine as the field of «children» is tremendous but it is worth using QUS as a side exam to help us in patient decision when needed and build awareness and confidence [69, 89, 90].
Are the manufacturer Intended use appropriate?
— The Sunlight Omnisense 7000/8000/MiniOmni Ultrasound Bone Sonometer is a non-invasive device that is designed for the quantitative measurement of the velocity of ultrasound waves («Speed of Sound» or «SOS» in m/sec) propagating along bones of adults and children. SOS provides a measure of skeletal fragility [91].
— The output is also expressed as a Z-score, and for adults also as a T-score, and can be used in conjunction with other clinical risk factors as an aid to the physician in the diagnosis of osteoporosis and other medical conditions leading to reduced bone strength and, ultimately, in the determination of fracture risk [91].
— The SOS measured by Omnisense 7000/8000/MiniOmni has a precision error low enough in comparison with the expected annual change in a patients’ measurement to make it suitable for monitoring bone changes which occur during the years of accelerated growth and in the early years following menopause (i.e., age range approximately 50–65 years) [91].
Based on the literature reviews, one can concluded that when use appropriately, following the good clinical practice and knowing the limitations of the clinical use, the Omnisense device is in conformity with its above specified Intended Use.
1. WHO. 1994. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Geneva, World Health Organization.
2. IOF Report 2008. Statistics and Facts.
3. Kanis J.A., Oden A., Johnell O. et al. The use of clinical risk factors enhances the performance of BMD in the prediction of hip and osteoporotic fractures in men and women // Osteoporos. Int. 2007; 18(8): 103346.
4. Kanis J.A., Burlet N., Cooper C. et al.; European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO). European guidance for the diagnosis and management of osteoporosis in postmenopausal women // Osteoporos. Int. 2008; Apr; 19(4): 399428. Epub 2008, Feb 12. Review. Erratum in: Osteoporos. Int. 2008 Jul; 19(7): 11034.
5. Njeh C.F., Hans D. Commercial Ultrasound Instrument // The evaluation of osteoporosis: Dual energy Xray and absorptiometry and ultrasound in clinical practice / Ed. by Blake G.M., Wahner H.W., Fogelman I. — Martin Dunitz Ltd, 1999. — P. 127146.
6. Krieg M.A., Barkmann R., Gonnelli S. et al. Quantitative ultrasound in the management of osteoporosis: the 2007 ISCD Official Positions // J. Clin. Densitom. 2008; 11(1): 163187.
7. Kung A.W., Wu C.H., Itabashi A. et al. International society for clinical densitometry official positions: Asiapacific region consensus // J. Clin. Densitom. 2010; 13: 34651.
8. Hans D., Kanis J.A., Baim S. et al. Joint Official Positions of the International Society for Clinical Densitometry and International Osteoporosis Foundation on FRAX(®). Executive Summary of the 2010 Position Development Conference on Interpretation and use of FRAX® in clinical practice // J. Clin. Densitom. 2011 JulSep; 14(3): 17180.
9. Moayyeri A., Adams J.E., Adler R.A. et al. Quantitative ultrasound of the heel and fracture risk assessment: an updated metaanalysis // Osteoporos. Int. 2012 Jan; 23(1): 14353. Epub 2011, Oct 27.
10. Sievänen H., Cheng S., Ollikainen S., UusiRasi K. Ultrasound velocity and cortical bone characteristics in vivo // Osteoporos. Int. 2001; 12: 399405.
11. Bossy E., Talmant M., Peyrin F. et al. An in vitro study of the ultrasonic axial transmission technique at the radius: 1MHz velocity measurements are sensitive to both mineralization and intracortical porosity // J. Bone Miner. Res. 2004 Sep; 19(9): 154856. Epub 2004, Jun 2.
12. Njeh C.F., Hans D., Wu C. et al. An in vitro investigation of the dependence on sample thickness of the speed of sound along the specimen // Medical Engineering & Physics. 1999; 21: 651659.
13. Wu C., Hans D., He Y. et al. Prediction of bone strength of distal forearm using radius bone mineral density and phalangeal speed of sound // Bone. 2000 May; 26(5): 529533.
14. Omnisense Series: FDA equivalent report 2011.
15. Hans D., Srivastav S.K., Singal C. et al. Does combining the results from multiple bone sites measured by a new quantitative ultrasound device improve discrimination of hip fracture? // J. Bone Miner. Res. 1999; 14: 64451.
16. Barkmann R., Kantorovich E., Singal C. et al. New method for quantitative ultrasound measurements at multiple skeletal sites // J of Clin. Densitom. 2000; 3: 17.
17. Weiss M., BenShlomo A., Hagag P., IshShalom S. Discrimination of proximal hip fracture by quantitative ultrasound measurement at the radius // Osteoporos. Int. 2000; 11: 41116.
18. Knapp K.M., Blake G.M., Spector T.D., Fogelman I. Multisite quantitative ultrasound: precision, age, and menopauserelated changes, fracture discrimination, and Tscore equivalence with dualenergy Xray absorptiometry // Osteoporos. Int. 2001; 12(6): 45664.
19. Njeh C.F., Saeed I., Grigorian M. et al. Assessment of bone status using speed of sound at multiple anatomical sites // Ultrasound Med. Biol. 2001 Oct; 27(10): 133745.
20. Knapp K.M., Blake G.M., Fogelman I. et al. Multisite quantitative ultrasound: Colles’ fracture discrimination in postmenopausal women // Osteoporos. Int. 2002; 13: 4749.
21. Damilakis J., Papadokostakis G., Vrahoriti H. et al. Ultrasound velocity through the cortex of phalanges, radius, and tibia in normal and osteoporotic postmenopausal women using a new multisite quantitative ultrasound device // Invest. Radiol. 2003 Apr; 38(4): 20711.
22. Hans D., Genton L., Allaoua S. et al. Hip Fracture Discrimination Study // J. Clin. Densitom. 2003; 6: 16372.
23. Damilakis J., Papadokostakis G., Vrahoriti H. et al. Ultrasound velocity through the cortex of phalanges, radius, and tibia in normal and osteoporotic postmenopausal women using a new multisite quantitative ultrasound device // Invest. Radiol 2003; 38: 20711.
24. Knapp K.M., Blake G.M., Spector T.D., Fogelman I. Can the WHO definition of osteoporosis be applied to multisite axial transmission quantitative ultrasound? // Osteoporos. Int. 2004; 15: 367374.
25. Damilakis J., Papadokostakis G., Perisinakis K. et al. Discrimination of hip fractures by quantitative ultrasound of the phalanges and the calcaneus and dual Xray absorptiometry // European Journal of Radiology 2004; 50: 26872.
26. Nguyen T.V., Center J.R., Eisman J.A. Bone mineral densityindependent association of quantitative ultrasound measurements and fracture risk in women // Osteoporos. Int. 2004; 15: 9427.
27. Clowes J.A., Eastell R., Peel N.F.A. The discriminative ability of peripheral and axial bone measurements to identify proximal femoral, vertebral, distal forearm and proximal humeral fractures: a case control study // Osteoporos. Int. 2005; 16: 1794802.
28. Boyanov M., Shinkov A., Nestorova R. Bone density measurement: quantitative ultrasound of the calcaneus and distal radius. A comparison with dual spectrum Xray absorptiometry // Dtsch Med. Wochenschr. 2007, Apr 20; 132(16): 86973.
29. Zhao Liang, Ren Sumei, Tang Hai, Luo Xiansheng. Assessment of the relationship between quantitative ultrasound measurement SOS (T) and hip BMD in population with and without osteoporotic fractures in the females.
30. Lin Hua, Bao Lihua, Han Zubin et al. Usefulness of DXA and QUS measurement in predicting vertebral fracture in osteoporotic patient.
31. Dobnig H., PiswangerSolkner J.C., ObermayerPietsch B. et al. Hip and nonvertebral fracture prediction in nursing home patients: role of bone ultrasound and bone marker measurements // J. Clin. Endocrinol. Metab. 2007, 92: 16781686.
32. Cook R.B., Curwen C., Tasker T., Zioupos P. Fracture toughness and compressive properties of cancellous bone at the head of the femur and relationships to noninvasive skeletal assessment measurements // Med. Eng. Phys. 2010 Nov; 32(9): 9917. Epub 2010, Jul 31.
33. Lee S.H., Khang Y.H., Lim K.H. et al. Clinical risk factors for osteoporotic fracture: a populationbased prospective cohort study in Korea // J. Bone Miner. Res. 2010 Feb; 25(2): 36978.
34. Olszynski W.P., Brown J.P., Adachi J.D. et al. Peripheral quantitative ultrasound for the prediction of fracture over five years: The Canadian Multicenter Osteoporosis Study (CaMOS). ECTS Conference proceeding. Athens, Greece, May 2011.
35. Weiss M., BenShlomo A.B., Hagag P., Rapoport M. Reference database for bone Speed of Sound Measurement by a Novel Quantitative Multisite Ultrasound Device // Osteoporosis International 2000; 11: 688696.
36. Drake W.M., McClung M., Njeh C.F. et al. Multisite Bone Ultrasound Measurement on North American Female Reference Population // Journal of Clinical Densitometry 2001; 4(3): 239248.
37. Hayman S.R., Drake W.M., Kendler D.L. et al. North American Male Reference Population for Speed of Sound in Bone at Multisite skeletal Sites // Journal of Clinical Densitometry 2002; 5(1): 6371.
38. Harris A.C., Doucette W.R., Reist J.C., Nelson K.E. Organization and results of student pharmacist bone mineral density screenings in women // J. Am. Pharm. Assoc. (2003). 2011 JanFeb; 51(1): 1004.
39. Cook R.B., Collins D., Tucker J., Zioupos P. Comparison of questionnaire and quantitative ultrasound techniques as screening tools for DXA // Osteoporos. Int. 2005; 16: 156575.
40. Tao B., Liu J.M., Li X.Y. et al. An assessment of the use of quantitative ultrasound and the Osteoporosis SelfAssessment Tool for Asians in determining the risk of nonvertebral fracture in postmenopausal Chinese women // J. Bone Miner. Metab. 2008; 26(1): 605. Epub 2008, Jan 10.
41. Korableva N.N. Life without Osteoporosis // New medical technologies magazine 2006, ISSN 16092163.
42. Paggiosi M.A., Clowes J.A., Finigan J. et al. Performance of quantitative ultrasound measurements of bone for monitoring raloxifene therapy // J. Clin. Densitom. 2010 OctDec; 13(4): 44150. Epub 2010, Sep 17.
43. BenShlomo A., Hagag P., Evans S., Weiss M. Early postmenopausal bone loss in hyperthyroidism // Maturitas 2001; 39: 1927.
44. Weiss M., BenShlomo P., Hagag P. et al. Effect of estrogen replacement therapy on speed of sound at multiple skeletal sites // Maturitas 2000; 35: 23743.
45. Segal E., Dvorkin N., Lavy A. et al. Bone density in axial and appendicular skeleton in patients with lactose intolerance: influence of calcium intake and vitamin D status // J. Am. Col. Nutr. 2003; 22: 2017.
46. Knapp K.M., Blake G.M., Spector T.D., Fogelman I. Differential effects of hormone replacement therapy on bone mineral density and axial transmission ultrasound measurements in cortical bone // Osteoporos. Int. 2003; 14: 28994.
47. Weiss M., KorenMichowitz M., Segal E., IshShalom S. Monitoring response to osteoporosis therapy with alendronate by a multisite ultrasound device // J. Clin. Densitom. 2003; 6: 21924.
48. Zadik Z., Sinai T., Borondukov E. et al. Longitudinal monitoring of bone accretion measured by quantitative multisite ultrasound (QUS) of bones in patients with delayed puberty (a pilot study) // Osteoporos. Int. 2005 Sep; 16(9): 103641. Epub 2004, Dec 23.
49. Böttcher J., Pfeil A., Mentzel H. et al. Peripheral bone status in rheumatoid arthritis evaluated by digital Xray radiogrammetry and compared with multisite quantitative ultrasound // Calcif. Tissue Int. 2006; 78: 2534.
50. Da Costa J.A., de Castro J.A., Foss M.C. The evaluation of renal osteodystrophy with cortical quantitative ultrasound at various bone sites // Ren. Fail. 2004 May; 26(3): 23741.
51. Tao B., Liu J.M., Zhao H.Y. et al. Differences between measurements of bone mineral densities by quantitative ultrasound and dualenergy Xray absorptiometry in type 2 diabetic postmenopausal women // J. Clin. Endocrinol. Metab. 2008 May; 93(5): 16705. Epub 2008, Mar 4.
52. Kang DougBong, Qiu Mingcal, Cao Ping, Liu Ping. Significance of ultrasound bone measurement in diagnosis of hyperthyroidism.
53. Blake G.M., Chinn D.J., Steel S.A. et al. A list of devicespecific thresholds for the clinical interpretation of peripheral Xray absorptiometry examinations // Osteoporos. Int. 2005; 16: 214956.
54. Hans D., Hartl F., Krieg M.A. Devicespecific weighted Tscore for two quantitative ultrasounds: operational propositions for the management of osteoporosis for 65 years and older women in Switzerland // Osteoporos. Int. 2003; 14: 25158.
55. Hans D., Durosier C., Kanis J. et al. Assessment of 10year probability of osteoporotic hip fracture combining clinical risk factors and heel bone ultrasound: The EPISEM prospective cohort of 12958 elderly women // J. Bone Miner. Res. 2008 Jul; 23(7): 104551.
56. Kanis J.A., Hans D., Cooper C. et al. Interpretation and use of FRAX in clinical practice // Osteoporos. Int. 2011 Sep; 22(9): 2395411. Epub 2011, Jul 21. Review.
57. Fuerst T., Hans D., Njeh C.F. Quality assurance in quantitative ultrasound // Quantitative ultrasound: osteoporosis and bone status assessment / Ed. by Njeh C.F., Hans D., Glüer C.C., Fuerst F., Genant H.K. — Martin Dunitz, 1999. — P. 163174.
58. Hans D., Bo F., Fuerst T. Non heel quantitative ultrasound devices // Quantitative ultrasound: osteoporosis and bone status assessment / Ed. by Njeh C.F., Hans D., Glüer C.C., Fuerst F., Genant H.K. — Martin Dunitz, 1999. — P. 145162.
59. Pfeil A., Böttcher J., Mentzel H.J. et al. Multisite quantitative ultrasound compared to dual energy Xray absorptiometry in rheumatoid arthritis: effects of body mass index and inflamed soft tissue on reproducibility // Rheumatol. Int. 2006 Oct; 26(12): 108490. Epub 2006, May 31.
60. Bianchi M.L., Baim S., Bishop N.J. et al. Official positions of the International Society for Clinical Densitometry (ISCD) on DXA evaluation in children and adolescents // Pediatr. Nephrol. 2010 Jan; 25(1): 3747.
61. Zemel B., Bass S., Binkley T. et al. Peripheral Quantitative Computed Tomography in Children and Adolescents: The ISCD 2007 Pediatric Official Positions // J. Clin. Densitom. 2008 JanMar; 11(1): 5974.
62. Nemet D., Dolfin T., Wolach B., Eliakim A. Quantitative Ultrasound Measurements of Bone Speed of Sound in Premature Infants // European Journal of Pediatric 2001; 160: 736740.
63. Eliakim A., Nemet D., Wolach B. Quantitative ultrasound measurements of bone strength in obese children and adolescents // J. Pediatr. Endocrinol. Metab. 2001 Feb; 14(2): 15964.
64. Zadik Z., Price D., Diamond G. Pediatric reference curves for multisite quantitative ultrasound and its modulators // Osteoporosis International. 2003 Oct; 14(10): 85762.
65. Hartman C., Brik R., Tamir A. et al. Bone quantitative ultrasound and nutritional status in severely handicapped institutionalized children and adolescents // Clin. Nutr. 2004 Feb; 23(1): 8998.
66. Zadik Z., Sinai T., Borondukov E. et al. Longitudinal Monitoring of Bone Accretion Measured by Quantitative Multisite Ultrasound (QUS) of Bone in Patients with Delayed Puberty (a pilot Study) // Osteoporosis International 2005; 16: 10361041.
67. Liao X.P., Zhang W.L., He J. et al. Bone measurements of infants in the first 3 months of life by quantitative ultrasound: the influence of gestational age, season, and postnatal age // Pediatr Radiol. 2005 Sep; 35(9): 84753.
68. Zadik Z., Sinai T., Zung A., Reifen R. Longitudinal monitoring of bone measured by quantitative multisite ultrasound in patients with Crohn’s disease. J Clin Gastroenterol. 2005 Feb;39(2):1203
69. Shchepliagina L.A., Somokhina E.O., Kruglova I.V., Chibrina E.A. Omnisense 7000 Ultrasound Bone sonometer: Benefits of Pediatric Use. Medical Business 3 (190). 2010
70. Liao X.P., Zhang W.L., He J.M. et al. Examination of infant bone status with quantitative ultrasound at birth // Zhonghua Er Ke Za Zhi. 2005 Feb; 43(2): 12832 (In Chinese).
71. Tomlinson C., McDevitt H., Ahmed S.F., White M.P. Longitudinal changes in bone health as assessed by the speed of sound in very low birth weight preterm infants // J. Pediatr. 2006 Apr; 148(4): 4505.
72. Pettinato A.A., Loud K.J., Bristol S.K. et al. Measurements in Adolescents and Young Adults. Effects of nutrition, puberty, and gender on bone ultrasound // Journal of Adolescent Health 2006; 39: 82834.
73. Ashmeade T., Pereda L., Chen M., Carver J.D. Longitudinal measurements of bone status in preterm infants // Journal of Perinatology 2007; 27: 693696.
74. McDevitt H., Tomlinson C., White M.P., Ahmed S.F. Changes in quantitative ultrasound in infants born at less than 32 weeks’ gestation over the first 2 years of life: influence of clinical and biochemical changes // Calcif. Tissue Int. 2007 Oct; 81(4): 2639.
75. Tshorny M., Mimouni F.B., Littner Y. et al. Decreased neonatal tibial bone ultrasound velocity in term infants born after breech presentation // J. Pediatr. Endocrinol. Metab. 2007 Mar; 20(3): 41524.
76. GökçeKutsal Y., Atalay A., SonelTur B. Effect of SocioEconomic Status on Bone Density in Children: Comparison of Two Schools by Quantitative Ultrasound Measurement // Journal of Pediatric Endocrinology & Metabolism 2007; 20: 5358.
77. Koo W.W., Bajaj M., Mosely M., Hammami M. Quantitative bone US measurements in neonates and their mothers // Pediatr. Radiol. 2008 Dec; 38(12): 13239.
78. Liao X.P., Zhang W.L., Yan C.H. et al. Reduced tibial speed of sound in Chinese infants at birth compared with Caucasian peers: the effects of race, gender, and vitamin D on fetal bone development // Osteoporos. Int. 2010 Dec; 21(12): 200311. Epub 2010, Feb 5.
79. Tansug N., Yildirim S.A., Canda E. et al. Changes in quantitative ultrasound in preterm and term infants during the first year of life // Eur. J. Radiol. 2010, Apr 1. Epub ahead of print.
80. Bajaj M., Koo W., Hammami M., Hockman E.M. Effect of subcutaneous fat on quantitative bone ultrasound in chicken and neonates // Pediatr. Res. 2010 Jul; 68(1): 813.
81. Christoforidis A., Economou M., Papadopoulou E. et al. Bone status of children with hemophilia A assessed with quantitative ultrasound sonography (QUS) and dual energy Xray absorptiometry (DXA) // J. Pediatr. Hematol. Oncol. 2010 Oct; 32(7): e25963.
82. Holmes B.L., Ludwa I.A., Gammage K.L. et al. Relative importance of body composition, osteoporosisrelated behaviors, and parental income on bone speed of sound in adolescent females // Osteoporos. Int. 2010 Nov; 21(11): 19537. Epub 2010, Jan 22.
83. Korakaki E., Damilakis J., Gourgiotis D. et al. Quantitative Ultrasound Measurements in Premature Infants at 1 Year of Age: The Effects of Antenatal Administered Corticosteroids // Calcif. Tissue Int. 2010, Dec 23. Epub ahead of print.
84. Koo W.W., Bajaj M., Hockman E.M., Hammami M. Bone ultrasound velocity in neonates with intrauterine growth deficit reflects a growth continuum // J. Clin. Densitom. 2011 JanMar; 14(1): 2832. Epub 2010, Nov 20.
85. Chen H.L., Lee C.L., Tseng H.I. et al. Assisted exercise improves bone strength in very low birthweight infants by bone quantitative ultrasound // J. Paediatr. Child Health. 2010 Nov; 46(11): 6539.
86. PereiradaSilva L., Costa A., Pereira L. et al. Early High Calcium and Phosphorus Intake by Parenteral Nutrition Prevents Shortterm Bone Strength Decline in Preterm Infants // J. Pediatr. Gastroenterol. Nutr. 2011 Feb; 52(2): 2039.
87. Maltsev S.V., Bogdanova A.V., Zotov N.A. Bone Status in adolescent of the Republic of Tatarstan. Medical alphabet // Radiology 2011; 1. ISSN 20785631.
88. Scheplyagina L.A., Samokhina E.O., Moisseva T.Yu. Qualitative Ultrasound Study in Children: Application of Sunlight Omnisense // Russian Journal of Pediatrics 2002; 6. ISSN 15609561.
89. Scheplyagina L.A., Rimarchuk G.V., Samokhina E.O. et al. Bone Strength in Children: known and unknown facts: Tutorial. — Moscow, 2011. ISBN 9785425301208.
90. Scheplyagina L.A., Rimarchuk G.V., Tyurina T.K. et al. Decrease of Bone Strength in Children with Chronic Gastroduodenitis: Tutorial. — Moscow, 2011. ISBN 9785425301192.
91. BeamMed Ltd. Omnisense QUS series Intents to use internal document. 2011.