Резюме
Мета дослідження: вивчити вплив регулярних аеробних фізичних навантажень інтенсивністю 6 балів за шкалою Борга на глікемічний профіль, чутливість до інсуліну, а також якiсть життя у пацієнтів iз цукровим діабетом (ЦД) 1-го типу. Матеріали і методи. Проаналізовано дані 42 пацієнтів iз ЦД 1-го типу — 20 жінок та 22 чоловікiв віком від 18 до 35 років (середній вік 25,3 ± 7,9 року). Рівень глікемії оцінювався портативним методом 6 разів на день. Дослідження вмiсту глікованого гемоглобіну проводилось імунотурбодиметричним методом. Для оцінки якості життя пацієнтів використовувався опитувальник Medical Outcomes Study Short Form 36 questionnaire. Результати. Доведено, що аеробні фізичні навантаження можуть значно модифікувати перебіг ЦД 1-го типу та змінювати якiсть життя. Через 30 днів регулярних аеробних фізичних навантажень у ранковий час середньодобова доза ультракороткого інсуліну зменшилася на 25,4 % від початкового рівня (р < 0,05). Виявлено, що чутливість до інсуліну при аеробних навантаженнях у хворих на ЦД 1-го типу збільшилася на 42,0 % (р < 0,05) та становила 0,60 ОД на 1 хлібну одиницю (ХО) наприкінці дослідження порівняно з 1,03 ОД на 1 ХО перед включенням пацієнтів у дослідження, а зниження рівня глікованого гемоглобіну становить у середньому 1,50 ± 0,12 % (р < 0,05). Установлено, що регулярні аеробні фізичні навантаження сприяють значному (p < 0,05) підвищенню рівня якості життя за шкалами як фізичного, так і психологічного компонента здоров’я (фізичне функціонування, рольове фізичне функціонування, інтенсивність болю, загальне здоров’я, рольове емоційне функціонування, життєва активність, психічне здоров’я, соціальне функціонування) порівняно з початковими показниками, що супроводжувалося підвищенням емоційної стійкості та працездатності. Висновки. Виявлено позитивний вплив регулярних аеробних фізичних навантажень на перебіг ЦД 1-го типу, а саме покращання глікемічного профілю, підвищення чутливості до інсуліну, а також якості життя пацієнтів.
Цель исследования: изучить влияние регулярных аэробных физических нагрузок интенсивностью 6 баллов по шкале Борга на гликемический профиль, чувствительность к инсулину, а также качество жизни у пациентов с сахарным диабетом (СД) 1-го типа. Материалы и методы. Проанализированы данные 42 пациентов с СД 1-го типа — 20 женщин и 22 мужчин в возрасте от 18 до 35 лет (средний возраст 25,3 ± 7,9 года). Уровень гликемии оценивался портативным методом 6 раз в день. Исследование содержания гликированного гемоглобина проводилось иммунотурбодиметрическим методом. Для оценки качества жизни пациентов использовался опросник Medical Outcomes Study Short Form 36 questionnaire. Результаты. Доказано, что аэробные физические нагрузки могут значительно модифицировать клиническое течение СД 1-го типа и изменять качество жизни. Через 30 дней регулярных аэробных физических нагрузок в утреннее время среднесуточная доза ультракороткого инсулина уменьшилась на 25,4 % от исходного уровня (р < 0,05). Выявлено, что чувствительность к инсулину при аэробных нагрузках у больных с СД 1-го типа увеличилась на 42,0 % (р < 0,05) и составила 0,60 ЕД на 1 хлебную единицу (ХЕ) в конце исследования по сравнению с 1,03 ЕД на 1 ХЕ перед включением пациентов в исследование, а снижение уровня гликированного гемоглобина составляет в среднем 1,50 ± 0,12 % (р < 0,05). Установлено, что регулярные аэробные физические нагрузки способствуют значительному (p < 0,05) повышению уровня качества жизни по шкалам как физического, так и психологического компонента здоровья (физическое функционирование, ролевое физическое функционирование, интенсивность боли, общее здоровье, ролевое эмоциональное функционирование, жизненная активность, психическое здоровье, социальное функционирование) по сравнению с исходными показателями, что сопровождалось повышением эмоциональной устойчивости и работоспособности. Выводы. Выявлено позитивное влияние регулярных аэробных физических нагрузок на течение СД 1-го типа, а именно улучшение гликемического профиля, повышение чувствительности к инсулину, а также качества жизни пациентов.
Background. The purpose of the study is to investigate the effect of regular aerobic physical exercises with 6-point intensity by Borg scale on glycemic profile, insulin sensitivity, and quality of life of patients with type 1 diabetes mellitus (DM). Materials and methods. The data from 42 patients with type 1 DM were analyzed. There were 20 women and 22 men aged 18 to 35 years (mean age 25.3 ± 7.9 years). The level of glycemia and glycated hemoglobin was estimated. The Medical Outcomes Study Short Form 36 questionnaire was used to assess the quality of life. Results. It has been shown that aerobic exercises can significantly modify the clinical course of type 1 DM and change the quality of life. After 30 days of regular aerobic exercises, the mean daily dose of ultra-short-acting insulin was decreased by 25.4 % versus baseline (p < 0.05). It was found that sensitivity to insulin after regular aerobic exercises was increased by 42.0 % and became 0.60 U per 1 bread unit (BU) by the end of the observation versus 1.03 U per 1 BU before the study. Also, regular physical activity was associated with the decrease in glycated hemoglobin content by 1.5 %. It has been established that regular aerobic exercises contributed to the significant (p < 0.05) increase in the quality of life according to all the scales which form physical and psychological components of health (physical functioning, role-physical functioning, bodily pain, general health, role-emotional functioning, vitality, mental health, social functioning) versus baseline that was accompanied by increase in emotional stability and workability. Conclusions. Regular aerobic exercises had the positive impact on the clinical symptoms of type 1 DM, resulted in improved glycemic profile, increased insulin sensitivity and quality of life of patients.
Introduction
After great increase in diabetes mellitus (DM) incidence in the 20th century, the term “non-infection epi–demy” has appeared, and this disease has become the global public health threat [1]. The high prevalence of DM determines its significance not only for the patients themselves and the health care system, but also for the society as a whole [8].
The most important task in the treatment of type 1 DM is to prevent microvascular complications, which are the main causes of disability in patients due to blindness, amputations and chronic kidney insufficiency. Only optimal glycemic control individually determined for each patient can prevent this [2].
Insulin therapy is one of the main ways for the best glycemic control in type 1 DM, but lifestyle modification is also important [6]. Most of the people with type 1 DM understand the role of diet, but compliance to the rules and guidelines is not absolute because of the ha–bits in–fluence, surroundings, and the problems in daily regimen. The third component for the optimal glycemic control is physical activity, although the role of this aspect in DM treatment is not often evaluated by patients and medical community [7].
In the number of studies, it has been proved that specific physical activity can significantly improve the control of DM [10, 12].
Unfortunately, such results were obtained only when special conditions were created that required a lot of time and effort from the patients, therefore, it could not be represented in the clinical practice.
At the same time, the question of possibility and effectiveness of physical exercises, its impact on the DM management, and the way the regular physical activity can modify the diabetes control are very topical.
The purpose of the research is to investigate the effect of regular aerobic physical exercises with 6-point intensity by Borg scale on glycemic profile, insulin sensitivity, and the quality of life (QL) of patients with type 1 diabetes mellitus.
Materials and methods
The data of 42 patients with type 1 DM were analyzed. There were 20 women and 22 men aged 18 to 35 years (mean age 25.3 ± 7.9 years). All patients included in the study had the compensated DM. Insulin therapy was administered with an ultra-short-acting insulin according to the dietary pattern and basal insulin.
The level of glycemia was measured 6 times a day — in the morning on an empty stomach, before and after aerobic exercise, and during the main meals.
Glycated hemoglobin (HbA1c) level was assessed on InnovaStar analyzer by immunoturbidimetric method. All patients included in the study performed aerobic exer–cises three times weekly.
The main requirements for physical activity were:
1) taking into account psychological characteristics of a patient;
2) all muscle groups must be involved;
3) no prolonged breaks and pauses;
4) duration 60 minutes or more;
5) energy expenditure at least 500 kcal per hour or more;
6) should be done in the morning.
According to these positions, the most convenient method to control the intensity of training was Borg scale. The main condition was individual and subjective load perception.
All subjects had moderate physical activity — 6 points by Borg scale, or 60.0–70.0 % of the highest possible heart rate. In this case, the simple and complex carbohydrates are the main resources for metabolism.
The team sports (25 patients) and swimming exer–cises (long, but not with maximum level, 17 patients) meet these requirements.
The Medical Outcomes Study Short Form 36 questionnaire (SF-36, developed and recommended by the International Center for Quality of Life Research) was used to assess the QL of patients. This questionnaire allows evaluating the subjective satisfaction of the patient with his physical and mental state, social functioning [11].
Patients were asked to fill the SF-36 questionnaire before the research and by the end of the controlled observation period. The SF-36 gives the opportunity to evaluate QL according to the eight scales: physical functioning (PF), role-physical functioning (RP), bodily pain (BP), general health (GH), vitality (VT), social functioning (SF), role-emotional functioning (RE) and mental health (MH) [11].
The patients had no previous history of smoking or drinking or gave up at least two weeks before the research. Dietary pattern included three main meals and two snacks.
Statistical analysis was performed using Statistica 7.0 (StatSoft, USA). Differences were statistically significant at p < 0.05.
Results
The clinical features of patients with type 1 DM before the study are presented in the Table 1.
After initial examination, the patients were included into prospective follow-up study (duration 25 to 37 days, the average of 32.50 ± 5.67 days).
The dynamics of ultra-short-acting insulin daily mean dose during controlled period is shown in Fig. 1.
The average insulin daily dose was calculated in accordance to individual observation chart for each patient during 2 weeks preceding the study and throughout the research period. As we can see, the mean daily dose of ultra-short-acting insulin was decreased from 35.1 ± 3.9 U to 28.00 ± 3.52 U (25.4 %, p < 0.05).
The basal bolus insulin doses did not change, with the mean of 19.20 ± 3.91 U/day. The bread units (BU) mean was 15.50 ± 2.71 and did not change before and after the study.
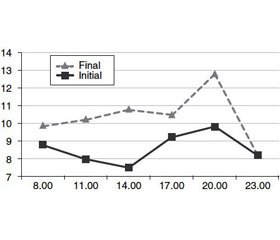
So, the sensitivity to insulin has significantly changed after regular aerobic exercises (Fig. 2).
As we can see, the sensitivity to insulin after regular aerobic exercises increased by 42.0 % and was 0.60 U per 1 BU by the end of the observation versus 1.03 U per 1 BU at baseline.
According to the received data, regular morning aerobic exercises induce two episodes of glycemic curve lowering. So, the reduction of glucose level occurred during physical activity and immediately after it, which may be not only due to the direct glucose utilization in response to aerobic exercises, but also the result of lower glucose level throughout the day.
The daily glycemic profile and its dynamics are shown in Fig. 3.
Also, it was interesting to mark the delayed, more pronounced, intense and prolonged glucose level reduction 3–4 hours after physical activity.
HbA1c is an indicator of glycemic control level, marker of DM compensation and relevance of hypoglycemic therapy.
In our work, after 30 days of controlled observation and regular physical exercises, there was a significant –decrease in the level of HbA1c that is shown in Fig. 4.
Thus, regular physical activity such as aerobic exer–cises in our study was associated with 1.5 % decrease in HbA1c.
During the first visit, SF-36 questionnaire [11] was also filled in.
The measuring model of the SF-36 has 3 levels: 1) the question; 2) eight scales, each of which consists of 2 to 10 points; 3) two aggregate measurements that combine the scales together. After analyzing the results, the answers have been received for all 36 items, which form 8 scales. Items are summed up and converted into values from 0 to 100 points, where 100 points is the maximum value, and 0 is the minimum. Higher scores represent the higher level of health.
The SF-36 includes one multi-item scale that asses–ses eight health concepts:
1. Physical functioning — limitations in physical activities because of health problems (self-service, walking, walking down the stairs, carrying weight, etc.).
2. Role limitation due to physical health is the influence of the physical state on the role functioning (work, daily activities).
3. Physical pain — the severity of pain and its impact on the ability to participate in everyday activities, including homework and out-of-home activities.
4. General health — assessing current state of health and the prospects for treatment.
5. Role limitation due to emotional problems implies an assessment of the extent of the emotional state interfering with work or other daily activities (including high time expenditures, reduced scope of work, decrease in its quality, etc.).
6. Vital energy means a feeling of full strength and energy or, conversely, the weakness.
7. Mental health characterizes the mood (presence of depression, anxiety, a general indicator of positive emotions).
8. Social functioning is determined by the extent of social activity (communication) restriction due to the physical or emotional state.
Scales are grouped into two indicators like “physical component of health” and “psychological component of health”:
I. Physical health. Components of the scale: 1) physical functioning; 2) role-playing function conditioned by physical condition; 3) pain intensity; 4) general health.
II. Psychological health component. Components of the scale: 1) mental health; 2) role-playing function conditioned by the emotional state; 3) social functioning; 4) life activity. Each item was used to process score only by one of the scales.
On the basis of 8 scales, the total assessment of physical and mental health was performed. SF-36 results are presented in Table 2.
It was found that QL decreased in all patients with –diabetes mellitus type 1 according to the all scales of SF-36 questionnaire. The lowest scores, when it was compared with the general population, were obtained on the scales of physical (PF, GH and RP) and psychological (RE, VT and SF) health components. Initial results indicate that physical and psychological health has a significant negative impact on routine activities.
The average indicators on the scales of role functioning conditioned by the emotional state, mental health, social functioning have shown that type 1 DM has a negative impact on the psychological component of health.
In the dynamics of treatment, it was found that the quality of life in patients with type 1 DM depends on the degree of glycemic compensation, as well as the level of physical activity. The reliable improvement of both physical and psychological components of health after regular morning aerobic exercises is proved.
Discussion
Physical activity is an important component of self-education that changes the level of compensation and quality of life in patients with type 1 DM.
Physical activity leads to increased insulin sensitivity and activation of non-insulin-sensitive glucose transporters (GLUT-4). Thus, physical activity in patients with type 1 DM may affect glycemia during some hours. The decrease in glycemia is related to the divergence between production and utilization of glucose [3, 9].
This one affects the suppressing level of insulin. In healthy people, in response to physical activity, suppression of insulin secretion and increased glucose production by the liver are proved. In patients with type 1 DM, the level of insulin can be corrected only in advance, and counterregulatory mechanisms are disturbed or absent [5].
Decreased glycemia in this period requires the correction of insulin therapy. This can be achieved by reducing ultra-short-acting insulin dosage, which was confirmed in our study. The second way is lowering the basal insulin dosage, which has to be studied in future.
Low level of physical activity is also associated with poor quality of life [4], so this aspect should be included in the education programs (“Diabetic schools”) to improve the patient’s social activity and adaptation.
Conclusions
We have revealed the positive effect of regular aerobic exercises on the clinical symptoms of type 1 diabetes mellitus resulted in the improved glycemic profile, increased insulin sensitivity and quality of life.
1. It has been shown that aerobic exercises can significantly modify the clinical course of type 1 diabetes mellitus and change the quality of life.
2. After 30 days of regular aerobic exercises, the mean daily dose of ultra-short-acting insulin is decreased by 25.4 % versus baseline (p < 0.05).
3. The sensitivity to insulin after regular aerobic exer–cises increased by 42.0 % and became 0.60 U per 1 BU by the end of the observation versus 1.03 U per 1 BU before the study.
4. Regular physical activity was associated with the decrease in glycated hemoglobin level by 1.5 %.
5. Regular aerobic exercises contributed to a significant (p < 0.05) improvement of the quality of life by all the scales, which form physical and psychological components of health (PF, RP, BP, GH, RE, VT, MH, SF) versus baseline.
Conflicts of interests. Authors declare the absence of any conflicts of interests that might be construed to influence the results or interpretation of their manuscript.
Список литературы
1. Резолюция ООН по сахарному диабету // Сахарный диабет. — 2007. — № 1. — С. 2-3.
2. Майоров А.Ю. Самоконтроль гликемии — основа эффективного лечения сахарного диабета / А.Ю. Майоров, О.Г. Мельникова, Ю.И. Филиппов // Эффективная фармакотерапия. — 2013. — № 35. — С. 46-56.
3. Acute bout of exercise induced prolonged muscle glucose transporter-4 translocation and delayed counter-regulatory hormone response in type 1 diabetes / K. Sato, T. Nishijima, T. Yokokawa et al. // PLoS One. — 2017. — Vol. 12(6). — e0178505; http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0178505
4. Association of olfactory function with the intensity of self-reported physical activity in adults with type 1 diabetes / B. Falkowski, M. Chudziński, E. Jakubowska et al. // Pol. Arch. Intern. Med. — 2017. — Vol. 127(7–8). — P. 476-480; http://pamw.pl/sites/default/files/KS_I_Falkowski.pdf
5. Clinical Outcomes to Exercise Training in Type 1 Diabetes: A Systematic Review and Meta-Analysis / D. Jewiss, C. Ostman, N. King et al. // Diabetes Res. Clin. Pract. — 2017. — Vol. 17. — P. 31108-31117; http://linkinghub.elsevier.com/retrieve/pii/S0168-8227(17)31108-7
6. Codella R. Why should people with type 1 diabetes exercise regularly? / R. Codella, I. Terruzzi, L. Luzi // Acta Diabetol. — 2017. — Vol. 54(7). — P. 615-630; https://link.springer.com/article/10.1007/s00592-017-0978-x
7. Delamater A.M. ISPAD Clinical Practice Consensus Guidelines 2014. Psychological care of children and adolescents with type 1 diabetes / A.M. Delamater, M. de Wit, V. McDarby // Pediatr. Diabetes. — 2014. — Suppl. 20. — P. 232-244.
8. Differential effects of age and sex on insulin sensiti–vity and body composition in adolescent offspring of women with type 1 diabetes: results from the EPICOM study / Z. Lohse, S. Knorr, B. Bytoft et al. // Diabetologia. — 2018. — Vol. 61(1). — P. 210-219; https://link.springer.com/article/10.1007%2Fs00125-017-4458-1
9. Interleukin-18 (rs187238) and glucose transporter 4 (rs5435) polymorphisms in Euro-Brazilians with type 1 diabetes / Y. Al-Lahham, A.K. Mendes, E.M. Souza // Genet. Mol. Res. — 2017. — Vol. 16(3); doi: 10.4238/gmr16039755.
10. Physical Activity Reduces Risk of Premature Morta–lity in Patients With Type 1 Diabetes With and Without Kidney Di–sease / H. Tikkanen-Dolenc, J. Wadén, C. Forsblom et al. // Diabetes Care. — 2017. — Vol. 40(12). — P. 1727-1732.
11. Ware J.E. SF-36 Health Survey. Manual and interpretation guide / J.E. Ware, K.K. Snow, M. Kosinski. The Health Institute, New England Medical Center. — Boston, Mass, 1993. — 28 p.
12. Yates T. Physical activity and type 1 diabetes: an underu–sed therapy / T. Yates, M.J. Davies // Diabet. Med. — 2017. — Vol. 34(11). — P. 1498-1499; http://onlinelibrary.wiley.com/doi/10.1111/dme.13445/epdf

/23-1.jpg)
/24-1.jpg)
/24-2.jpg)